Tα λεμφώματα είναι καρκίνοι των κυττάρων του λεμφικού συστήματος και κυρίως των λεμφοκυττάρων.
Εμφανίζονται όταν ένα
αναπτυσσόμενο λεμφοκύτταρο παρουσιάσει κάποιο γενετικό λάθος
(μετάλλαξη). Αυτή η μετάλλαξη το οδηγεί είτε να πολλαπλασιάζεται πιο
γρήγορα από το φυσιολογικό, είτε να ζει περισσότερο απ’ ό,τι έπρεπε,
χωρίς να ανταποκρίνεται στους κανονικούς φυσιολογικούς ελέγχους.
Το λέμφωμα είναι ο πιο συνηθισμένος αιματολογικός καρκίνος και ο τρίτος πιο συχνός καρκίνος στα παιδιά.
Σύμφωνα με τον Όμιλο Εθελοντών κατά του Καρκίνου «Αγκαλιάζω», υπάρχουν δύο είδη λεμφωμάτων, τα Hodgkin’s (HL) και τα non Hodgkin’s (NHL) λεμφώματα, με πολλές διαφορετικές κατηγορίες (έξι κατηγορίες Hodgkin’s και τουλάχιστον 61 non Hodgkin’s). Τα λεμφώματα Hodgkin’s διαφέρουν από τα non Hodgkin’s στον τρόπο που αναπτύσσονται, στον τρόπο με τον οποίο εισβάλλουν στους γειτονικούς ιστούς και στην αγωγή που χρησιμοποιείται για την καταπολέμηση τους.
Ανάλογα με την ταχύτητα με την οποία αναπτύσσονται τα non Hodgkin’s, χαρακτηρίζονται ως:
- Επιθετικά ενδιαμέσου/υψηλού βαθμού
- Βραδείας εξέλιξης – χαμηλού βαθμού
Παράγοντες κινδύνου ανάπτυξης λεμφώματος είναι οι εξής:
- Οικογενειακό ιστορικό
- Αυτοάνοσα νοσήματα
- Μεταμόσχευση
- Έκθεση σε χημικά, όπως φυτοφάρμακα, για μεγάλα χρονικά διαστήματα.
- Μόλυνση από ιούς, όπως ο Epstein-Barr (που προκαλεί τη λοιμώδη μονοπυρήνωση), HTLV-1, HIV/AIDS, ηπατίτιδα C, ή και κάποια βακτήρια, όπως το ελικοβακτηρίδιο (που προκαλεί έλκος)
Στο σημείο αυτό πρέπει να τονιστεί ότι το να έχεις κάποιον παράγοντα κινδύνου δεν σημαίνει πως κατ’ ανάγκη θα αναπτύξεις λέμφωμα. Στην πράξη, οι περισσότεροι άνθρωποι με παράγοντες κινδύνου δεν εμφανίζουν λέμφωμα. Αντιθέτως, οι περισσότεροι ασθενείς με λέμφωμα δεν έχουν εκτεθεί σε κανένα γνωστό παράγοντα κινδύνου.
Παρ’όλο που δεν είναι γνωστό γιατί αναπτύσσονται τα λεμφωματα, γνωρίζουμε πως δεν είναι δυνατό να οφείλονται σε τραυματισμό και πως δεν είναι μεταδοτικά.
Τα συμπτώματα αυτά είναι:
- Διόγκωση των λεμφαδένων σε λαιμό, μασχάλες, τράχηλο, βουβωνική περιοχή
- Πυρετός, ειδικά το βράδυ
- Ρίγη ή αλλαγές στην θερμορύθμιση
- Ανεξήγητη απώλεια βάρους
- Απώλεια όρεξης
- Ασυνήθιστη κόπωση η έλλειψη ενέργειας
- Αναιμία
- Επίμονος βήχας
- Δυσκολία στην αναπνοή
- Επίμονος κνησμός (φαγούρα) σε ολόκληρο το σώμα χωρίς εμφανή αιτία
- Γενικευμένη κούραση
- Διογκωμένες αμυγδαλές
- Πονοκέφαλοι
- Διόγκωση ήπατος και/ή σπλήνα
Η κλινική εξέταση μπορεί να αποκαλύψει διογκωμένους λεμφαδένες σε διάφορες περιοχές του σώματος. Ο γιατρός προχωρεί σε εξετάσεις αίματος και βιοψία ενός διογκωμένου λεμφαδένα, κατά την οποία ο λεμφαδένας μελετάται στο παθολογοανατομικό εργαστήριο για να ταυτοποιηθεί η νόσος.
Μετά την ταυτοποίηση του, ακολουθεί μια σειρά εργαστηριακών εξετάσεων για να εντοπιστούν τα σημεία της νόσου (στάδιο νόσου). Αυτές οι εξετάσεις μπορεί να είναι:
- Απλές αιματολογικές εξετάσεις
- Απεικονιστικές εξετάσεις (τομογραφία, μαγνητική κ.ά.) ώστε να εντοπιστούν τυχόν άλλοι λεμφαδένες και να ελεγχθεί το συκώτι, ο σπλήνας ή οι πνεύμονες
Ανάλογα με την κρίση του γιατρού, ίσως χρειαστούν πιο ειδικές εξετάσεις, όπως παρακέντηση του μυελού των οστών.
- Στάδιο II: Περιλαμβάνει πάνω από μία περιοχή λεμφαδένα σε μια πλευρά του διαφράγματος ή μια ζώνη λεμφαδένα και μια κοντινή περιοχή ή όργανο.
- Στάδιο III: Περιλαμβάνει ζώνες λεμφαδένων και στις δύο πλευρές του διαφράγματος και ένα όργανο η μία περιοχή πλησίον των λεμφαδένων, τον σπλήνα η κάποιο άλλο όργανο ή περιοχή.
- Στάδιο IV: Περιλαμβάνει ένα η περισσότερα όργανα και τον μυελό των οστών ή το δέρμα.
Συνήθως τα λεμφώματα αντιμετωπίζονται με χημειοθεραπεία, ακτινοθεραπεία, βιολογική θεραπεία, με κάποιο συνδυασμό αυτών, μεταμόσχευση ή απλή παρακολούθηση.
Για τα βραδέως εξελισσόμενα NHL μπορεί να μη δοθεί αρχικά κάποια θεραπεία. Είναι η λεγόμενη τακτική «παρατήρηση και αναμονή» («watch and wait»). Εάν δεν υπάρχουν συμπτώματα, ο γιατρός μπορεί να προτιμήσει τη στενή παρακολούθηση του ασθενούς και να δώσει τη θεραπεία όταν πραγματικά θα χρειάζεται.
Το λέμφωμα είναι ο πιο συνηθισμένος αιματολογικός καρκίνος και ο τρίτος πιο συχνός καρκίνος στα παιδιά.
Σύμφωνα με τον Όμιλο Εθελοντών κατά του Καρκίνου «Αγκαλιάζω», υπάρχουν δύο είδη λεμφωμάτων, τα Hodgkin’s (HL) και τα non Hodgkin’s (NHL) λεμφώματα, με πολλές διαφορετικές κατηγορίες (έξι κατηγορίες Hodgkin’s και τουλάχιστον 61 non Hodgkin’s). Τα λεμφώματα Hodgkin’s διαφέρουν από τα non Hodgkin’s στον τρόπο που αναπτύσσονται, στον τρόπο με τον οποίο εισβάλλουν στους γειτονικούς ιστούς και στην αγωγή που χρησιμοποιείται για την καταπολέμηση τους.
Ανάλογα με την ταχύτητα με την οποία αναπτύσσονται τα non Hodgkin’s, χαρακτηρίζονται ως:
- Επιθετικά ενδιαμέσου/υψηλού βαθμού
- Βραδείας εξέλιξης – χαμηλού βαθμού
Πρόληψη – Παράγοντες κινδύνου
Παρ’ όλο που τα πραγματικά αίτια των λεμφωμάτων παραμένουν άγνωστα, ορισμένοι κοινοί παράγοντες φαίνονται να επηρεάζουν τον κίνδυνο εμφάνισης. Η νόσος είναι πιο συχνή σε άτομα με εξασθενημένο ανοσοποιητικό σύστημα, καθώς και σε άτομα που εκτίθενται σε περιβαλλοντικά καρκινογόνα, φυτοφάρμακα, ζιζανιοκτόνα, ιούς και ορισμένα βακτήρια.Παράγοντες κινδύνου ανάπτυξης λεμφώματος είναι οι εξής:
- Οικογενειακό ιστορικό
- Αυτοάνοσα νοσήματα
- Μεταμόσχευση
- Έκθεση σε χημικά, όπως φυτοφάρμακα, για μεγάλα χρονικά διαστήματα.
- Μόλυνση από ιούς, όπως ο Epstein-Barr (που προκαλεί τη λοιμώδη μονοπυρήνωση), HTLV-1, HIV/AIDS, ηπατίτιδα C, ή και κάποια βακτήρια, όπως το ελικοβακτηρίδιο (που προκαλεί έλκος)
Στο σημείο αυτό πρέπει να τονιστεί ότι το να έχεις κάποιον παράγοντα κινδύνου δεν σημαίνει πως κατ’ ανάγκη θα αναπτύξεις λέμφωμα. Στην πράξη, οι περισσότεροι άνθρωποι με παράγοντες κινδύνου δεν εμφανίζουν λέμφωμα. Αντιθέτως, οι περισσότεροι ασθενείς με λέμφωμα δεν έχουν εκτεθεί σε κανένα γνωστό παράγοντα κινδύνου.
Παρ’όλο που δεν είναι γνωστό γιατί αναπτύσσονται τα λεμφωματα, γνωρίζουμε πως δεν είναι δυνατό να οφείλονται σε τραυματισμό και πως δεν είναι μεταδοτικά.
Συμπτώματα
Είναι πολύ σημαντικό ο καθένας μας να γνωρίζει τα συμπτώματα του λεμφώματος, διότι μπορεί να σώσει τη ζωή του. Τα συμπτώματα μπορεί να μοιάζουν με αυτά λιγότερο επικίνδυνων ασθενειών και για αυτόν τον λόγο η διάγνωση είναι μερικές φορές δύσκολη. Από την άλλη, η έγκαιρη διάγνωση είναι πολύ σημαντική, διότι ορισμένες επιθετικές μορφές μπορεί να είναι θανατηφόρες σε μικρό χρονικό διάστημα. Αναγνωρίζοντας λοιπόν νωρίς τα συμπτώματα υπάρχουν καλύτερες προοπτικές για γρηγορότερη διάγνωση, αγωγή και επιβίωση.Τα συμπτώματα αυτά είναι:
- Διόγκωση των λεμφαδένων σε λαιμό, μασχάλες, τράχηλο, βουβωνική περιοχή
- Πυρετός, ειδικά το βράδυ
- Ρίγη ή αλλαγές στην θερμορύθμιση
- Ανεξήγητη απώλεια βάρους
- Απώλεια όρεξης
- Ασυνήθιστη κόπωση η έλλειψη ενέργειας
- Αναιμία
- Επίμονος βήχας
- Δυσκολία στην αναπνοή
- Επίμονος κνησμός (φαγούρα) σε ολόκληρο το σώμα χωρίς εμφανή αιτία
- Γενικευμένη κούραση
- Διογκωμένες αμυγδαλές
- Πονοκέφαλοι
- Διόγκωση ήπατος και/ή σπλήνα
Διάγνωση
Οι περισσότεροι άνθρωποι που παραπονιούνται για τέτοια συμπτώματα δεν έχουν λέμφωμα. Παρ’ όλα αυτά, είναι πολύ σημαντικό εάν κάποιος έχει συμπτώματα που δεν υποχωρούν, να επισκεφτεί τον γιατρό ώστε να επιβεβαιώσει ότι δεν πάσχει από λέμφωμα ή κάποια άλλη σοβαρή ασθένεια.Η κλινική εξέταση μπορεί να αποκαλύψει διογκωμένους λεμφαδένες σε διάφορες περιοχές του σώματος. Ο γιατρός προχωρεί σε εξετάσεις αίματος και βιοψία ενός διογκωμένου λεμφαδένα, κατά την οποία ο λεμφαδένας μελετάται στο παθολογοανατομικό εργαστήριο για να ταυτοποιηθεί η νόσος.
Μετά την ταυτοποίηση του, ακολουθεί μια σειρά εργαστηριακών εξετάσεων για να εντοπιστούν τα σημεία της νόσου (στάδιο νόσου). Αυτές οι εξετάσεις μπορεί να είναι:
- Απλές αιματολογικές εξετάσεις
- Απεικονιστικές εξετάσεις (τομογραφία, μαγνητική κ.ά.) ώστε να εντοπιστούν τυχόν άλλοι λεμφαδένες και να ελεγχθεί το συκώτι, ο σπλήνας ή οι πνεύμονες
Ανάλογα με την κρίση του γιατρού, ίσως χρειαστούν πιο ειδικές εξετάσεις, όπως παρακέντηση του μυελού των οστών.
Στάδια λεμφώματος
- Στάδιο I: Περιλαμβάνει μία μόνο ζώνη η περιοχή, συχνά ένα μόνο λεμφαδένα και την περιβάλλουσα περιοχή. Τυπικά δεν παρουσιάζονται συμπτώματα.- Στάδιο II: Περιλαμβάνει πάνω από μία περιοχή λεμφαδένα σε μια πλευρά του διαφράγματος ή μια ζώνη λεμφαδένα και μια κοντινή περιοχή ή όργανο.
- Στάδιο III: Περιλαμβάνει ζώνες λεμφαδένων και στις δύο πλευρές του διαφράγματος και ένα όργανο η μία περιοχή πλησίον των λεμφαδένων, τον σπλήνα η κάποιο άλλο όργανο ή περιοχή.
- Στάδιο IV: Περιλαμβάνει ένα η περισσότερα όργανα και τον μυελό των οστών ή το δέρμα.
Θεραπεία
Τα λεμφώματα είναι δυνητικά ιάσιμη νόσος. Ο αιματολόγος μπορεί να συστήσει αρκετούς τύπους θεραπειών ή και απλή παρακολούθηση, ανάλογα με τα ιδιαίτερα χαρακτηριστικά της νόσου.Συνήθως τα λεμφώματα αντιμετωπίζονται με χημειοθεραπεία, ακτινοθεραπεία, βιολογική θεραπεία, με κάποιο συνδυασμό αυτών, μεταμόσχευση ή απλή παρακολούθηση.
Για τα βραδέως εξελισσόμενα NHL μπορεί να μη δοθεί αρχικά κάποια θεραπεία. Είναι η λεγόμενη τακτική «παρατήρηση και αναμονή» («watch and wait»). Εάν δεν υπάρχουν συμπτώματα, ο γιατρός μπορεί να προτιμήσει τη στενή παρακολούθηση του ασθενούς και να δώσει τη θεραπεία όταν πραγματικά θα χρειάζεται.

What Is It?
Non-Hodgkin's lymphoma is cancer that starts in your body's lymph system. There are a lot of different kinds, and even doctors can have a hard time telling them apart. While it's typically found in older adults, it's still one of the more common cancers in children. It's not always easy to spot, but great strides in finding and treating it means the outlook now is better than ever.

The Lymph System
Think of it as the body's cleaning service. Lymph is a watery liquid that flows between cells and clears out the stuff they don't need anymore. It's carried around in tubes that connect to lymph nodes, which are small bean-shaped filters. These trap waste and germs and help get them out of your body. You have clusters of nodes in your armpits, belly, groin, neck, and pelvis.
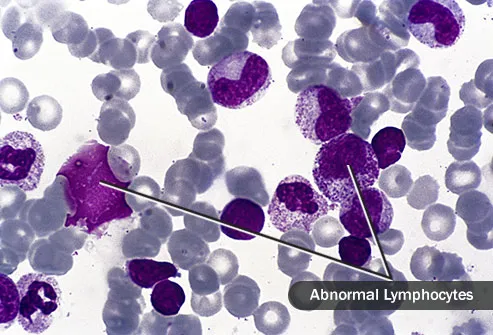
Lymphocytes
This is where it starts, with these white blood cells. Lymphocytes called B cells point out germs, and T cells destroy them. When these disease-fighters are done, they should die off. But with non-Hodgkin's lymphoma, they grow and divide out of control. As you get more and more of them, your lymph nodes may start to swell. Most often, it's in the B cells where things go wrong.

Early Symptoms
The most common is a swollen lymph node, usually in your armpit, groin, or neck. But these can be painless and easy to overlook. Lymph nodes can also swell when you're fighting an infection, so they're easy to shrug off.
You might also have a fever that won't go away, night sweats that soak your clothes, and weight loss for no reason, and you may be extremely tired.

Symptoms Based on Where It Is
The lymph system runs throughout the body, so lymphoma can appear almost anywhere. In your stomach, you might throw up or feel full after even a small meal. Lymphoma can make your skin itchy or give you red bumps. When it's in your chest, it can hurt and cause trouble breathing. The key is to notice when something's off and check in with your doctor.

Types of NHL
There are more than 30 kinds of non-Hodgkin's lymphomas. They differ by whether it starts in B or T cells, how the cells look, and what kinds of genes and proteins they have. Doctors also look at how fast the cancer grows and spreads. Slow ones are called indolent; faster ones, aggressive. Diffuse large B-cell lymphoma is the most common type. It typically comes on in your 60s. It's aggressive but can be cured.
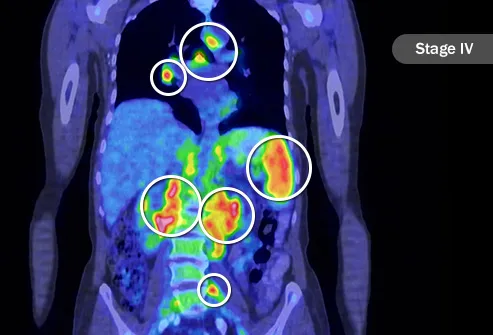
Staging
Your cancer's stage has a big impact on choosing the best treatment. It tells you how advanced the cancer is. At stage I, it's in just one area of lymph nodes. Or it's in one of the lymph system organs, like the tonsils. By stage IV, it's in lymph nodes above and below your diaphragm. That's the thin muscle that separates your chest and belly. It's also in other organs like your liver or lungs.

Staging Letters
An A with the number (as in stage IA) means you have no symptoms.
B means you have fever, night sweats, or have lost some weight.
E stands for extranodal, which means the cancer has spread to tissue just outside some lymph nodes.
An X, also called bulky disease, means you have at least one tumor that's larger than 10 centimeters (about 4 inches, or roughly the width of your palm).
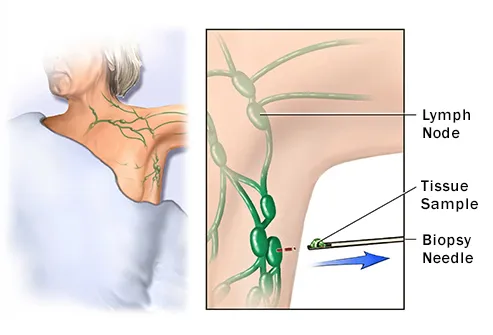
Biopsy
This test tells you for sure if you have cancer. Your doctor removes a swollen lymph node, or part of one, for testing. The doctor who looks at the tissue may be able to tell what type of non-Hodgkin's lymphoma you have, too. This is important because your treatment depends on it. But doctors who have less experience with lymphoma can and do get the test results wrong. If you have doubts, ask for a second opinion from a specialist.

Other Tests
These can help your doctor figure out the stage of your lymphoma as well as check on how well your treatment is working. Imaging, like a CT, PET, or MRI scan, looks for traces of cancer in lymph nodes and other parts of your body. Your doctor might do a bone marrow biopsy (taking a sample from your hipbone or breastbone with a needle) to see if cancer has spread into the soft, spongy inner part. You'll likely get blood tests, too.

Wait-and-See Approach
For a slow-growing lymphoma in the early stages, the best treatment may be no treatment at all. These types could go for years without causing any problems. That doesn't mean you ignore it, though. You'll still have regular checkups so you and your doctor can keep a close eye on things. If you have symptoms or it's a more aggressive type, you'll likely need care right away.

Chemotherapy
This common treatment uses medicine to kill cancer cells. You typically get it through pills or an IV, though you could also get a shot. You may also get more than one drug. Each chemo medicine attacks cancer in a different way, so using several can be very effective. Because the drugs act throughout your body, they may cause side effects like hair loss, throwing up, and a higher chance of infections.

Stem Cell Transplant
High-dose chemotherapy can knock out more cancer, but it also wipes out bone marrow, which is where blood cells are made. That's where this treatment comes in. First, your doctor removes and saves some of your young blood cells, called stem cells. (You can also get stem cells from a donor.) When you're finished with chemo, those saved (or new) cells are put into your body to make up for what was lost. It's also called a bone marrow transplant.

Immunotherapy
These treatments rally your immune system to attack the lymphoma. One approach is to use medications called monoclonal antibodies that glom on to cancer cells. They're like signs that say, "These cells are bad! Get rid of them!" And your body takes it from there. Another method uses antibodies with radiation in them. Once they lock onto a cancer cell, the radiation destroys it.

Targeted Therapy
Cancer cells work differently from normal cells. Targeted drugs take advantage of those differences. For example, proteasome inhibitors keep cancer cells from dividing. Kinase inhibitors get in the way of proteins that help cancer cells grow and thrive. Basically, targeted therapies attack only the cancer and spare your healthy cells. The side effects are often less severe than with chemotherapy.

Radiation Therapy
High-energy beams focus on the cancer to kill it. For an early-stage non-Hodgkin's lymphoma, this may be the only treatment you need. More often though, it's used along with something else, like chemotherapy. Each session lasts only few minutes and doesn't hurt. You typically get it 5 days a week for several weeks.

Survival Rates
Your outlook depends on a lot of things, like the type and stage, as well as your age and overall health. Generally speaking though, for non-Hodgkin's lymphoma, the 5-year relative survival rate is 70%. That means compared to every 10 people who don't have NHL, on average, seven people with NHL are still alive after 5 years. The 10-year relative survival rate is 60%. Keep in mind these numbers are not your story.

After Treatment
Even in the best case, when a cure is possible, cancer takes a toll. The disease is challenging physically and emotionally. You may worry about it coming back. It affects your work life and maybe your finances. This is where a survivorship care plan may help. It's a tool you and your doctors can use to map out what comes next. Yes, it's about follow-ups and tests, but it covers your emotional well-being, too.

Causes
In most cases, doctors just don't know. Age plays a role -- it's most common in people 60 and older. Things that weaken your immune system may raise your odds as well, like a condition you're born with, an organ transplant, or infections including HIV and bacteria related to stomach ulcers called H. pylori. There also seem to be links to chemicals used on insects and weeds, but we need more research.

Prevention
There's really not much you can do. Even the things that we know raise your chances are largely out of your control. It isn't simply a matter of healthy eating, though that can't hurt. Likewise, there's no test to find it early on. The best you can do is keep your eye out for symptoms. And if your risk is greater, keep up with your regular doctor's appointments.
SOURCES :WebMD , ONMED.GR














































